Slide 2: A variety of approaches
exist for the treatment of obsessive-compulsive disorder (OCD). Four
major approaches include psychodynamic, cognitive-behavioral,
humanistic, and family systems. Each approach perceives obsessive
compulsive disorder as an intrusive condition characterized by unwanted
repetitive and anxiety-producing thoughts accompanied by the compulsive
act of rituals the individual believes will protect them from the
anxiety (Hansell & Damour, 2008). The obsessions are thoughts or
impulses over which the individual has no control except to apply the
ritual for relief, and the compulsions make the individual feel driven
to do something - usually the ritualistic practice for the purpose of
relieving the anxiety (Hansell & Damour, 2008).
OCD
has a well-established biological component similar to other anxiety
disorders. According to the National Institutes of Health (2010)
anxiety produces affective physical reactions in people, and the
biological perspective views the activation or stimulation of the
nervous system and its excesses or deficiencies. There may also be
associated genetic predispositions, neuro-chemical, and hormonal
malfunctions (Schimelpfening, 2009). Emotion components include
underlying concerns or experiences that have not been openly addressed.
From a psychodynamic perspective, there may be pain and sadness
resulting from early childhood parental relations. Most psychologists
consider underlying conditions as a prelude to OCD (Hansell &
Damour, 2008).
The
cognitive-behavioral components of OCD include cognitive distortions of
oneself and one's environment. Anxiety is often the result of
maladaptive thought processes and dysfunctional thought patterns.
Misinterpreted situations, and the underestimation of emotional ability
may contribute to the disorder. As mentioned previously, behavioral
components include the obsessive thoughts or impulses which precedes the
application of ritualistic practice (Hansell & Damour, 2008). Each
approach has distinct perceptions of OCD and equally distinct methods
of management.
Freud
also theorized the symptoms of OCD were caused by misunderstood
punishment and rigid toilet training that led to internalized conflicts.
Other psychodynamic theorists considered OCD the result of the
cultural demand for cleanliness and neatness, as well as parental style
and punishment tactics during childhood. According to Fraum (2011),
"the fundamental issues that drive these symptoms include fear of
rejection or abandonment, as well as interpersonal issues regarding
intimacy, sex, control, power or other problems in their relationship"
(para. 11). Freud published a case study on a patient he called
Rat-man. He claimed he successfully treated the man for obsessive
thoughts and compulsive behaviors which Freud thought began from sexual
and punitive issues in his childhood (Wertz, 2003).
The
goal of the psychodynamic interventions is to help clients understand
the roots of their symptoms, gain greater self-acceptance, develop
better solutions to emotional conflicts, and decrease needs for
problematic defense mechanisms (Hansell & Damour, 2008). In the
case of OCD by relieving individuals’ stress, they will cease to need to
use the defense mechanism.
According to Abend (1996), psychodynamic
therapy focuses on pathological anxiety that arises from unconscious
emotional conflicts, so therapists in this discipline tend to use basic
psychodynamic techniques to address most anxiety disorders (Abend,
1996). Through an established bond between the patient and the
therapist, the patient is encouraged to speak freely to uncover the
roots of the anxiety, and to recall dreams. Guided imagery and movement
is also used in the psychodynamic approach. The therapist helps the
client identify and understand problems as a reaction to present and
past issues.
Since
the psychodynamic approach seeks to uncover unconscious directives, the
therapist must be capable of interpreting the patient's thoughts,
feelings, and dreams and assisting the patient to identify the
unconscious motives to help the patient resolve the conflicting
emotions. A significant part of psychodynamic therapy is the ongoing
bond built between the patient and the therapist and the trust within
the relationship will allow the patient to thoroughly investigate the
issues.
Uncovering
the roots of anxiety is effective in any anxiety disorder and
psychodynamic therapy has been successfully used in the development of
treatment goals, as well as, especially in group treatment (Wells,
Glickauf-Hughes, & Buzzell, 1990). The patients modify their
character by “evolving autonomous functions and partly through evolving
relationships with other individuals” (Wells, Glickauf-Hughes, &
Buzzell, 1990, p. 375). According to Bram and Björgvinsson ( 2004), in
severe cases of OCD cognitive behavioral therapy was more successful
than psychodynamic therapy alone and relieved more symptoms of the OCD.
Bram and Björgvinsson ( 2004) claim that training psychodynamic
clinicians to accommodate cognitive-behavioral techniques will help
successfully treat patients with OCD.
In
a cognitive behavioral intervention, the goal would be to change the
way the individual responds to the stimulus in effect, changing the
ritualistic response to the disturbing thoughts. For example, a client
may be asked to allow themselves to think about the disturbing thoughts
without engaging in the usual ritualistic behavior. According to
Hansell and Damour (2009), the goal of cognitive-behavioral therapy
would be to interrupt the ritualistic behavior to allow the client to
experience the dissipation of the anxiety even without the application
of the ritual. When the process of obsessive thoughts followed by
ritualistic behavior is interrupted, the behavior ceases to negatively
reinforce the anxiety, so the pattern is broken.
Cognitive
therapists teach strategies and perspectives for responding to the
challenges that life has to offer so that individuals can gain a greater
sense of self-efficacy (i.e. developing faith in their abilities to
achieve specified goals). Equally as important as knowledge, training,
experience, and credentials on the part of the cognitive therapist are
warmth, understanding, and compassion (Phillipson, n.d., para. 3).
Cognitive interventions for anxiety
disorders are generally goal-oriented and highly structured; cognitive
therapists take an active, directive stance toward the client and his or
her problems (Beck, Emery, & Greenberg, 2005). The therapist will
help the client identify the automatic responses to the disturbing
thoughts, and the negativity associated with the thoughts. They might
discuss the logic (or lack thereof) of the disturbing thoughts and
identify the distortions involved in such thinking. Ultimately, the
client will be taught how to challenge his or her typical thought
processes.
Because
the cognitive- behavioral perspective is based on the idea that people
learn from reinforcement from the environment, the strategies in
therapeutic application emphasize altering the pattern of reinforcement.
If a response causes disordered patterns, a change in response is
necessary (Phillipson, n.d.). The behaviorist approach claims all
learning takes place by the organisms adaptability to change according
to its environment, and changing that response alters the established
pattern.
Research
(Clark et al., 2003) finds cognitive-behavioral therapy effective in
treating anxiety disorders. According to Phillipson (n.d.), cognitive
behavioral treatment for obsessive-compulsive disorder provides the
client with effective tools with which to continually manage anxiety and
challenge internalized thinking. Rather than depending on a therapist
for longer periods, the client can immediately learn to use the
cognitive-behavioral tools. The behavioral tools are ultimately
important in the client's ability to continue the management of the
disturbing thoughts, and finally decrease the endless ritualizing.
Nathan and Gorman (2002) found the interventions were as effective used
alone as in combination with other behavioral techniques such as
relaxation training.
The
goal of humanistic therapy for OCD is to create an appropriate
environment by which the patient will be able to develop, mature, and
evolve, and as a result continue the process in healthy development
(Dombeck, 2006). I the humanistic view, psychological dysfunction is
caused by an interruption in development because of social and emotional
immaturity. By enabling natural development, the patient regains his
or her natural ability to proceed in a healthier direction. By
maintaining natural development, individuals continue along their
personal life pathway, and meeting their psychological needs.
One
well-known Gestalt technique is known as the empty chair technique
which is a visualization technique wherein the patient is directed to
imagine a person in the empty chair that sits in the therapists office.
By entering into a discussion with the imagined person, conflicts are
more easily resolved. The goal is to allow the patient to work with the
fears and emotions surrounding the issue, ultimately rendering the
situation less scary whereby the patient no longer needs to avoid the
other person or situation (Dombeck, 2006).
According
to Whelton (2004), depth of experience in psychotherapy is positively
related to outcome. In humanistic therapy, this depth is a normal
expectation and one goal of its application. This indicates feelings
and emotions are being processed and new more appropriate meanings are
formed as well as finding solutions to problems that create fear and
avoidance, and other issues that derail the natural human proclivity to
evolve. There is, however, no empirical research clarifying the
effective role of humanistic therapy in relieving the intrusive symptoms
of obsessive -compulsive disorder.
Family
systems approaches differ from psychodynamic, behavioral, and
humanistic approaches as they use the integration of the family in
recognizing and treating disordered emotions and behavior. Rather than
working with the individual having the specific problem, the whole
family is involved in the therapy. Psychological insight provided a new
platform for therapy that supported the family as an interrelated
system, not a group composed of members with random, unrelated
experiences. Rather than viewing the identified individual as affected
by motivations exclusive of the family, this new systems saw the
identified individual as a product of the family unit and "dysfunction
resided in the family as an interrelated system" (Plante, 2011, p. 60).
The
goal of family systems therapy is to treat the whole family and reduce
the dysfunction affecting all the members, but more severely expressed
by the identified family member. The issues of the identified
individual are acknowledged and addressed, although within the scope of
the family. As well as developing the identified individual, the system
also develops each family member as autonomous and independent while
re-establishing family solidarity (Plante, 2011). The system seeks a
balance between the function of the group and the independent individual
performance.
In family systems the therapist
guides the family in assessing their needs and defining goals.
Improving communication within the group is accomplished by several
techniques including reframing or changing perceptions within the group,
and paradoxical intention, which defines symptoms, especially those of
OCD to alleviate resistance to the therapy. Joining or developing a
rapport with the family allows the therapist to become more familiar
with the mechanisms by which the OCD became symptomatic. Through
establishing rapport with the family unit, the therapist can identify
any anxiety producing relationships or psychological enmeshment between
members (Plante, 2011). Furthermore, the therapist assists in the
recognition of disengagement of one or more members whereby the
individuals remove themselves from the family unit as a coping
mechanism, in this case the symptoms of disturbed thoughts and
ritualistic coping behavior. Alleviating the symptoms of OCD in one
family member includes understanding the anxiety and psychological
pressure the individual experiences. Identifying such issues will help
to establishing new ways of relating within the family, disabling the
individual's need for obsessive-compulsive behaviors.
The
communication approach seeks to re-establish healthy communication
within the family thereby eliminating unreasonable expectations,
inappropriate rules, and inaccurate assumptions between the individuals,
which may be causing the OCD symptoms. The structural approach aims to
disengage dysfunctional family patterns and balance relationships,
while the Milan approach establishes the therapist as an integral member
of the family, providing a neutral position and garnering respect for
the unit. The guidelines of all the specific techniques and strategies
embrace the general assumption that the family unit contains the
dysfunction causing the OCD, and issues are not exclusive to the
identified individual (Plante, 2011).
Unlike
the other three approaches addressed herein, family systems therapy
addresses inadequacies in the family unit. Although addressing these
relational issues, there is little evidence that family systems therapy
is efficient as an exclusive therapy for treating OCD. Carr (2000)
believes family therapy is an effective treatment "either alone or as
part of a multimodal or multisystemic treatment program for child abuse
and neglect, conduct problems, emotional problems, and psychosomatic
problems" (p. 48) although severe symptoms of OCD requires adjunct
therapy.
The major theoretical approaches
are philosophies about human behavior that provide psychologists with a
thematic conceptual understanding of mental health, illness, and
disorder. The approaches also provide a consistent parameter by which
to assess and treat the patient and a dependable plan of action in a
variety of situations and patient needs. Whereas the psychodynamic
perspective emphasizes the unconscious directives that influence the
individual's ability to maintain normal functioning, the foundation of
the cognitive-behavioral approach focuses on contemporary, measurable
and observable behavior. It uses classical and operant conditioning as
explanations for many types of behavior.
The
humanistic approach emphasizes the natural human ability to evolve and
develop and perceives people as "active, thinking, creative, and growth
oriented" (Plante, 2011, p. 133) and crave self-actualization. The
family systems approach views the unhealth of the individual as a
consequence of dysfunction in the family, and only by creating health
and solidarity within the family can the individual be freed from
symptoms of mental illness.
Psychologist
have become more integrating with their perspective preference and less
rigid to one particular theoretical approach. Each approach has
advantages for specific challenges, and some perspectives lend
themselves to particular research whereas others do not. The
integration of various theoretical perspectives in clinical psychology
allows the therapist to afford the broadest potential for successful
change within the individual. "Furthermore, as more research and
clinical experience help to uncover the mysteries of human behavior,
approaches need to be adapted and shaped in order to best accommodate
these new discoveries and knowledge" (Plante, 2011, p. 132). The human
psyche is a rich and complex maze of diverse needs and challenges,
served most appropriately by an equally elaborate and divergent palette
of treatments and interventions.
Abend, S. M. (1996). Psychoanalytic psychotherapy. In C. Lindemann
(Ed.), Handbook of the treatment of anxiety disorders (pp. 401–410). Northvale, NJ: Jason Aronson, Inc.
Allacentric. (n.d.). [Sisyphus]. Retrieved August 13, 2011, from http://www.seekersdigest.org/?p=920
Beck,
A. T., Emery, G., & Greenberg, R. L. (2005). Anxiety disorders
and phobias: A cognitive perspective. Cambridge, MA: Basic Books.
Bram,
A., & Björgvinsson, T. (2004). A psychodynamic clinician's foray
into cognitive-behavioral therapy utilizing exposure-response prevention
for obsessive-compulsive disorder. American Journal of Psychotherapy,
58(3), 304-320.
Carr,
A. (2000). Evidence-based practice in family therapy and systemic
consultation Child-focused problems. Journal of Family Therapy, 22(1),
29-60. doi: 10.1111/1467-6427.00137
Clark,
D. M., Ehlers, A., McManus, F., Hackmann, A., Fennell, M., Campbell,
H., ... Louis, B. (2003). Cognitive therapy versus fluoxetine in
generalized social phobia: a randomized placebo-controlled trial.
Journal of Consulting and Clinical Psychology, 71(6), 1058-1067. doi:
10.1037/0022-006X.71.6.1058
Dombeck,
M. (2006). Humanistic Psychotherapy. Mental Health, Depression,
Anxiety, Wellness, Family & Relationship Issues, Sexual Disorders
& ADHD Medications. Retrieved August 12, 2011, from
http://www.mentalhelp.net/poc/view_doc.php?type=doc
Freud
Museum Vienna. (2006). [Freud]. Retrieved August 14, 2011, from
http://www.glogster.com/glog.php?glog_id=14323765&scale=54&isprofile=true
Fraum, R. M. (2002). Obsessive Compulsive Disorder. Psychotherapy and Counseling for Obsessive Compulsive Disorder (OCD). Retrieved August 15, 2011, from http://www.psychologistcounselorpsychotherapist.com/obsessive-compulsive-disorder-ocd-nyc-westchester.aspx
Fraum, R. M. (2002). Obsessive Compulsive Disorder. Psychotherapy and Counseling for Obsessive Compulsive Disorder (OCD). Retrieved August 15, 2011, from http://www.psychologistcounselorpsychotherapist.com/obsessive-compulsive-disorder-ocd-nyc-westchester.aspx
Glogster.
(n.d.). [OCD Graphic]. Retrieved August 14, 2011, from
http://www.glogster.com/glog.php?glog_id=14323765&scale=54&isprofile=true
Hands
On Network. (2011). [Family]. Retrieved August 13, 2011, from
http://handsonblog.org/2010/07/06/6-ways-family-volunteering-benefits-businesses
Hansell, J., & Damour, L. (2008). Abnormal psychology. Hoboken, NJ: Wiley.
Nathan, P. E., & Gorman, J. M. (2002). A guide to treatments that work (2nd ed.). New York: Oxford University Press.
National
Institutes of Health. (2010). Anxiety Disorders: MedlinePlus. National
Library of Medicine - National Institutes of Health. Retrieved August
13, 2011, from http://www.nlm.nih.gov/medlineplus/phobias.html
Per
Caritatem. (2011). [Human Graphic]. Retrieved August 15, 2011, from
http://percaritatem.com/2011/02/19/part-i-fanon-and-foucault-on-humanism-and-rejecting-the-%E2%80%9Cblackmail%E2%80%9D-of-the-enlightenment/
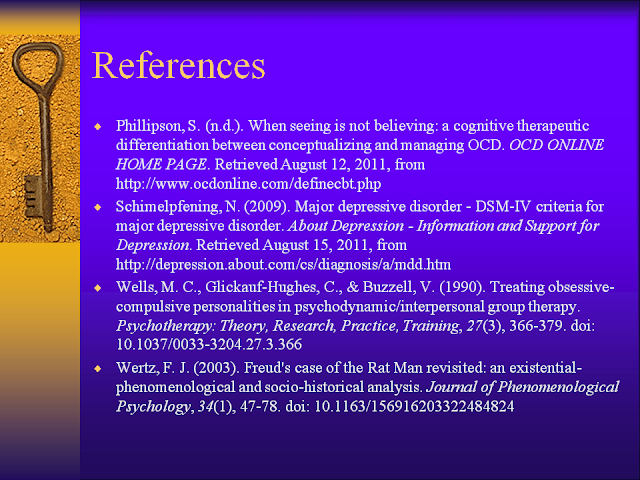
¨Phillipson,
S. (n.d.). When seeing is not believing: a cognitive therapeutic
differentiation between conceptualizing and managing OCD. OCD ONLINE
HOME PAGE. Retrieved August 12, 2011, from
http://www.ocdonline.com/definecbt.php
Schimelpfening,
N. (2009). Major depressive disorder - DSM-IV criteria for major
depressive disorder. About Depression - Information and Support for
Depression. Retrieved August 15, 2011, from
http://depression.about.com/cs/diagnosis/a/mdd.htm
Wells,
M. C., Glickauf-Hughes, C., & Buzzell, V. (1990). Treating
obsessive-compulsive personalities in psychodynamic/interpersonal group
therapy. Psychotherapy: Theory, Research, Practice, Training, 27(3),
366-379. doi: 10.1037/0033-3204.27.3.366
Whelton, W. J. (2004). Emotional processes in psychotherapy: evidence across therapeutic modalities. Clinical Psychology & Psychotherapy, 11(1), 58-71. doi: 10.1002/cpp.392